---
tags: 名詞解釋
---
# 心律變異分析(HRV)
1. **簡述**:
一種==量測連續心跳速率變化程度==的方法,利用心跳速度的變化作為指標,間接了解自律神經的活性狀態。
2. [**臨床應用**](http://www.westgarden.com.tw/medicenter_gallery/%E5%82%BE%E8%81%BD%E9%AB%94%E5%85%A7%E6%B7%B1%E5%B1%A4%E7%9A%84%E8%81%B2%E9%9F%B3-%E8%87%AA%E5%BE%8B%E7%A5%9E%E7%B6%93%E6%AA%A2%E6%B8%AC%E5%84%80%E4%B9%8B%E8%87%A8%E5%BA%8A%E6%87%89%E7%94%A8%E8%A5%BF/):
> 當心率變異數值愈差,未來罹患或死於心血管疾病的機率愈高。
- 當心率變異不正常,代表自律神經功能不好,也反映可能隱藏著的身心不健康。
- 預測發生心血管疾病病人的長期存活率
- 可做為個人整體健康情形的重要指標,可適用對象為不明原因失眠、心悸、胸悶、倦怠、頭暈、腸胃不適等族群
3. **測量器具**:
- 一台可以測量脈搏的儀器

- UNISAGE HRV檢測儀(台灣本土的寰碩公司所研發製造)
## [心律變異度(HRV) 名詞介紹](https://zh.m.wikipedia.org/zhtw/%E5%BF%83%E7%8E%87%E8%AE%8A%E7%95%B0%E5%88%86%E6%9E%90):
### Time Domain
| 指標 | 單位 | 說明 |
| -------- | -------- | -------- |
| SDNN | ms | 正常心跳間期的標準差 |
| SDANN index | ms | 計算短時間的平均正常心跳間期,通常是5分鐘,<br>然後再計算全程的平均標準偏差 |
| R-MSSD | ms | 正常心跳間期差值平方根的均方根 |
| NN50 | 個 | 正常心跳間期差值超過50毫秒的個數 |
| PNN50 | % | 相鄰正常心跳間期差值超過50毫秒的比例 |
### [**Frequency Domain** :](http://www.vicon.com.tw/zh-tw/a4-646-1188/%E5%8E%9F%E7%90%86.html)
> 利用==離散傅立葉變換==將心跳間隔的時間序列轉換為頻域。一般心率變異訊號的頻譜分析使用200至500連續心跳間期穩定記錄表現,因此記錄需要數分鐘的時間。主要為==高頻區(HF 0.15-0.40赫茲)及低頻區(LF 0.04-0.15赫茲)==。高頻區通常反映副交感神經的活性,低頻區同時受到交感與副交感神經系統的調控。
| 指標 | 單位 | 說明 |
| -------- | -------- | -------- |
| TP | ms^2 | 擷取之頻率為 <= 0.4hz |
| HF | ms^2 | 擷取之頻率為 0.15 - 0.4hz<br>指高頻範圍的正常心跳間期的變異數 |
| LF | ms^2 | 擷取之頻率為 0.04 - 0.15hz<br>指低頻範圍的正常心跳間期的變異數 |
| VLF | ms^2 | 擷取之頻率為 0.003 - 0.04hz<br>指極低頻範圍的正常心跳間期的變異數 |
| ULF | ms^2 | 擷取之頻率為 <= 0.003hz<br>指超極低頻範圍的正常心跳間期的變異數 |
| LF/HF | None | 反應交感/副交感神經平衡的指標或代表交感神經調控的指標 |
## HRV與疾病的關係
https://www.joiiup.com/knowledge/content/1781
(下面有論文連結)
==HRV可用於評估自律神經失衡,疾病和死亡率。副交感神經活動低下和HRV異常已經證實與免疫功能障礙和身體發炎有關,其涉及包括心血管疾病、糖尿病、骨質疏鬆症、關節炎、阿茲海默症和牙周病在內的各種疾病某些類型的癌症,以及肌力下降、虛弱和殘疾增加[3,13]==
==Kloter團隊的研究[14]發現較高的HRV與癌症患者的疾病進展和結果呈正相關。具有較高HRV和先進應對機制的患者在癌症進展中具有更好的預後。研究人員認為HRV是了解癌症患者總體健康狀況的有用參數。==
==被列為可改變的其他三個可被視為生活方式因素(lifestyle factors),包括吸煙、缺乏運動(鍛煉)和肥胖。兩個不可改變的危險因素是年齡和有早期心臟病或中風的家族史。值得注意的是,有許多數據顯示,**這些風險因素中的每一個都與HRV低下有關。**==
==***心率變異性和預防心血管疾病***
有一些途徑可以通過它們來防止或最小化可改變因素,如工作壓力的有害影響。所有這些途徑都涉及增加HRV。而戒菸、運動和減重已被證實是心率變異性(HRV)增加的有效方法。膳食結構的改變包括食用水果和蔬菜,適量飲酒,以及通過魚類或堅果食用攝入omega-3脂肪酸和維生素D等也是有效的途徑,這些方法與HRV增加都有一些證據連結==
==HRV降低與幾種心理狀況和狀態有關。心理社會因素,如充滿壓力的生活事件、壓力、敵意、抑鬱和焦慮也成為心血管疾病的危險因素。與心血管疾病和HRV相關的另一個新興社會心理因素是工作壓力。==
在男性造船廠工作人員的一項研究中,發現在高壓力工作組中,SDNN顯著降低。重要的是,代謝症候群也與高壓力工作組中SDNN降低顯著相關。因此,高壓力工作組交感神經過度活動和低HRV相結合可能是與心臟病發作相關的潛在心血管功能障礙的有用指標。這也是Vrijkotte研究團隊在一個白領階層的研究的發現。其中一個主要結果是睡眠時心率的一個SD增加或ln RMSSD (RMSDD的自然對數) 的一個SD減少與輕度高血壓的風險顯著增加有關。
==這些結果表明,促進交感神經支配的慢性干擾可能是工作壓力對心血管疾病風險影響的一個重要原因。結論是HRV可以成為研究工作壓力及其伴隨生理影響的非常有用的工具。許多研究已經證實,工作壓力與冠心病(CHD)風險增加有關。==
:bulb:==簡言之,心率變異性(HRV)的減少作為與各種慢性疾病,行為障礙,死亡率和衰老相關的風險的預後指標已受到越來越多的關注。==
## HRV與疾病的關係的論文
> 論文名稱:Normal Values of Corrected Heart-Rate Variability in 10-Second Electrocardiograms for All Ages
[論文1連結](https://www.researchgate.net/publication/324803116_Normal_Values_of_Corrected_Heart-Rate_Variability_in_10-Second_Electrocardiograms_for_All_Ages)
> 論文名稱:Heart rate variability and first cardiovascular event in populations without known cardiovascular disease: Meta-analysis and dose-response meta-regression
[論文2連結](https://www.researchgate.net/publication/235391742_Heart_rate_variability_and_first_cardiovascular_event_in_populations_without_known_cardiovascular_disease_Meta-analysis_and_dose-response_meta-regression)
> 論文名稱:The Impact of Resonance Frequency Breathing on Measures of Heart Rate Variability, Blood Pressure, and Mood
[論文3連結](https://www.frontiersin.org/articles/10.3389/fpubh.2017.00222/full)
HRV偏低與糖尿病、心血管風險 [論文1、論文2]
HRV與疾病相關的重要論文
[1] Friedman BH, Thayer JF. Autonomic balance revisited: panic anxiety and heart rate variability. J Psychosom Res 1998;44:133–51.
[2] Kang MG, Koh SB, Cha BS, Park JK, Woo JM, Chang SJ. Association between job stress on heart rate variability and metabolic syndrome in shipyard male workers. Yonsei Med J 2004;45:838–46.
[3] Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R. Emotions, morbidity, and mortality: new perspectives from psychoneuroimmunology. Annu Rev Psychol 2002;53: 83–107.
[4] Duijts SF, Kant I, Swaen GM, van den Brandt PA, Zeegers MP. A meta-analysis of observational studies identifies predictors of sickness absence. J Clin Epidemiol 2007;60:1105–15.
[5] Harter JK, Schmidt FL, Hayes TL. Business-unit-level relationship between employee satisfaction, employee engagement, and business outcomes: a meta-analysis. J Appl Psychol 2002;87:268–79.
[6] Rosengren A, Hawken S, Ounpuu S, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:953–62.
[7] Chandola T, Britton A, Brunner E, et al. Work stress and coronary heart disease: what are the mechanisms? Eur Heart J 2008;29:640–8.
[8] Murray CJL, Lopez AD. The global burden of disease: a comprehensive assessment of mortality and disability from disease injuries and risk factors in 1990 and projected to 2002. Boston, MA: Harvard School of Public Health; 1996.
[9] Yusuf S, Reddy S,Ounpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 2001;104:2746–53.
[10] Darwin C. The expression of emotion in man and animals. New York: Oxford University Press; 1998.
[11] Friedman BH, Thayer JF. Anxiety and autonomic flexibility: a cardiovascular approach. Biol Psychol 1998;49:303–23.
[12] Malliani A, Pagani M, Lombardi F. Methods for assessment of sympatho-vagal balance: power spectral analysis. Armonk, New York: Futura; 1994.
[13] Ershler WB, Keller ET. Age-associated increased interleukin-6 gene expression, late-life diseases, and frailty. Annu Rev Med 2000;51:245–70.
[14] Evelyne Kloter, et al, Heart Rate Variability as a Prognostic Factor for Cancer Survival – A Systematic Review, Frontier on Physiology, May 2018, Vol.9, Article 623.
[15] Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. European Heart Journal (1996) 17, 354–381
[16] Kleiger RE, Miller JP, Bigger Jr JT, Moss AJ. Decreased heart rate variability and its association with increased mortality after acute myocardial infarction. Am J Cardiol 1987;59:256–62.
[17] Tsuji H, Venditti Jr FJ, Manders ES, et al. Reduced heart rate variability and mortality risk in an elderly cohort. The Framingham Heart Study. Circulation 1994;90:878–83.
[18] Liao D, Carnethon M, Evans GW, Cascio WE, Heiss G. Lower heart rate variability is associated with the development of coronary heart disease in individuals with diabetes: the atherosclerosis risk in communities (ARIC) study. Diabetes 2002;51:3524–31.
[19] La Rovere MT, Bigger Jr JT, Marcus FI, Mortara A, Schwartz PJ. Baroreflex sensitivity and heart-rate variability in prediction of total cardiac mortality after myocardial infarction. ATRAMI (autonomic tone and reflexes after myocardial infarction) investigators. Lancet 1998;351:478–84.
[20] Fang, S. C., Wu, Y. L., & Tsai, P. S. (2020). Heart Rate Variability and Risk of All-Cause Death and Cardiovascular Events in Patients With Cardiovascular Disease: A Meta-Analysis of Cohort Studies. Biological Research for Nursing, 22(1), 45-56.
[21] Mozaffarian D, Stein PK, Prineas RJ, Siscovick DS. Dietary fish and omega-3 fatty acid consumption and heart rate variability in US adults. Circulation 2008;117:1130–7.
[22] Park SK, Tucker KL, O'Neill MS, et al. Fruit, vegetable, and fish consumption and heart rate variability: the Veterans Administration Normative Aging Study. Am J Clin Nutr 2009;89:778–86.
[23] Brosschot JF, Gerin W, Thayer JF. The perseverative cognition hypothesis: a review of worry, prolonged stress-related physiological activation, and health. J Psychosom Res 2006;60:113–24.
[24] Tiller WA, McCraty R, Atkinson M. Cardiac coherence: a new, noninvasive measure of autonomic nervous system order. Altern Ther Health Med 1996;2:52–65.
[25] Macleod J, Davey Smith G, Heslop P, Metcalfe C, Carroll D, Hart C. Psychological stress and cardiovascular disease: empirical demonstration of bias in a prospective observational study of Scottish men. BMJ 2002;324:1247–51.
[26] Vrijkotte TG, van Doornen LJ, de Geus EJ. Effects of work stress on ambulatory blood pressure, heart rate, and heart rate variability. Hypertension 2000;35:880–6.
[27] Belkic KL, Landsbergis PA, Schnall PL, Baker D. Is job strain a major source of cardiovascular disease risk? Scand J Work Environ Health 2004;30:85–128.
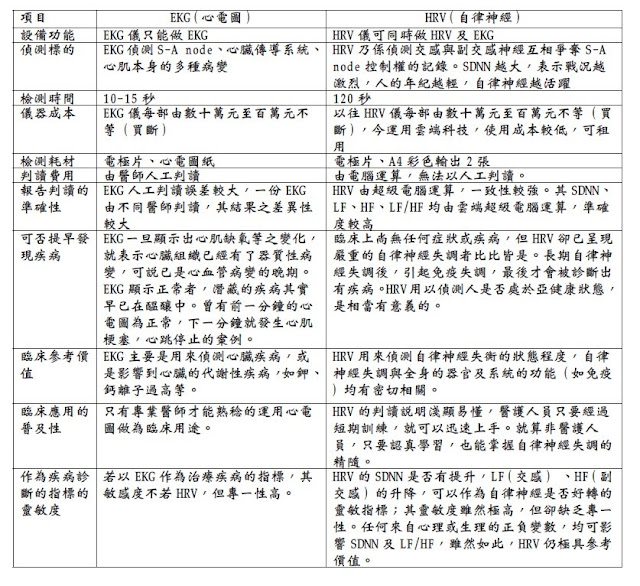
## [自律神經(HRV)檢測 vs 心電圖(EKG)](http://hrvtw.blogspot.com/2010/09/hrv_13.html):
- 自律神經(HRV)檢測的方法與做心電圖(EKG)原理步驟方法完全一致,做出來的同樣都是心電圖,只是==解讀此心電圖的角度、分析重點==不同而已。
- EKG是根據心電圖的形態(Morphplogy)、結構來判定
ex:竇房結(S-A node)、房室結(A-V node)、房室束、普金氏纖維有無阻滯異常;心肌有無病變、壞死、肥大以及心軸有無偏移
- HRV則是對同樣一份心電圖(EKG),另外一種角度的判讀,經由觀測自律神經對竇房結(S-A node)調控的程度來判定人的自律神經生理活性(時域:SDNN)及交感副交感強度(頻域:LF、HF)
- 比較表: